Just a migraine?
Case courtesy of Dr. Macey Yates Johnson
Presentation
A 50-year-old woman with history of migraines, hypertension, and chronic neck pain presents to the emergency department by EMS with complaint of headache and syncope. She was recently diagnosed with COVID last week and feels generally weak. Today, she was with family and had a syncopal episode, where her family helped her to the ground and there was no trauma. EMS reports that on scene she was slightly hypotensive with SBP in the high 90s with blood glucose within normal limits. She was also noted to be slightly confused on scene which was not her baseline; stroke scale was negative.
Patient denies chest pain, shortness of breath, fevers, but reports she has a history of migraines and had worsening headaches since one week ago. Four days ago she experienced the “worst headache of her life” and it has persisted. She states that she has had multiple falls over the past week due to weakness. She denies any blood thinner use.
On initial presentation, the patient is afebrile with other vitals within normal limits. Exam demonstrates a lethargic-appearing woman who answers questions appropriately but does appear to be slightly confused. Otherwise, neuro exam is nonfocal and NIHSS is 0. The is no evidence of trauma, and exam is otherwise unremarkable
Workup/ED Course
EKG was without evidence of acute ischemia or arrhythmia. Chest x-ray was grossly unremarkable.
Labs did not demonstrate any significant leukocytosis, anemia, or metabolic derangement. Lactate was within normal limits.
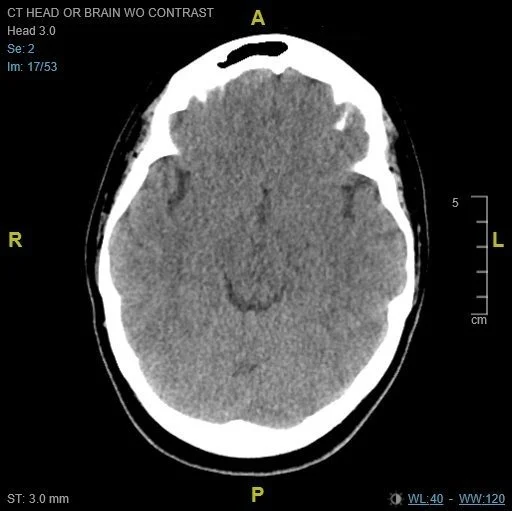
CT Head Radiology Impression:
“1. Focal subarachnoid hemorrhage in the posterior left frontal lobe.
2. Low-density in the occipital lobes bilaterally may represent cortical contusions, ischemic infarctions, or encephalopathy. Recommend MRI for further evaluation.”
A CT of the head demonstrated a small subarachnoid hemorrhage in the left frontal lobe with multiple occipital infarcts bilaterally. A CTA head/neck obtained was grossly unremarkable for aneurysm or other vascular abnormality.
Neurology was consulted and recommended admission and MRI imaging without LP or empiric meningitis treatment. Neurosurgery was also consulted and made aware of the patient's intracranial hemorrhage. The patient was admitted to the ICU for further work-up and management.
Outcome
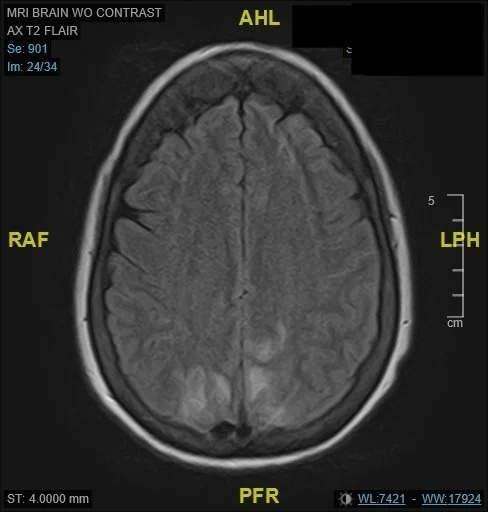
MRI Brain Radiology Impression: “Relatively symmetric T2 lengthening related to the parieto-occipital regions, with possibly a small amount of diffusion restriction, and cortical subarachnoid hemorrhage. The appearance is suggestive of posterior reversible encephalopathy syndrome and/or reversible cerebral vasoconstriction syndrome.”
An MRI was obtained, with findings as above, concerning for posterior reversible encephalopathy syndrome and/or reversible cerebral vasoconstriction syndrome.
While admitted, the patient had progressive weakness and altered mental status requiring intubation. A Transcranial Doppler was performed which showed evidence of vasospasm. This prompted repeat CT angiography which demonstrated multiple regions of vasospasm. This was thought to be related to a prescription for a triptan medication which the patient had been prescribed for her migraines.
Based on these findings the patient was taken for an urgent angiography where she received verapamil intra-arterially. She eventually was extubated, showed significant improvement in weakness, and had improvement in mental status. She was discharged to a skilled nursing facility after starting Verapamil with instructions to discontinue triptan use.
The patient’s final diagnosis was determined to have been SAH secondary to PRES with superimposed RCVS, in the setting of recent COVID-19 infection and triptan medication use.
Takeaway Points
When evaluating patients with chronic migraines, avoid anchoring upon chronic conditions and perform a thorough evaluation, including imaging if indicated
Vasospasm can be caused by triptan medications often prescribed for migraines
While rare, cases of PRES have been reported in association with COVID-19
Thanks again to Dr. Yates Johnson for this interesting case!
Have a cool case that you would like to share? Please email thomas.rauser@uhsinc.com or scan the QR codes in the conference room or TVH ED. Cases will be written with provider anonymity unless consent is given otherwise.